How It Started …
Three years ago I started to get knee pain. I went to a sports and exercise doctor who I had been seeing for a glute med problem and, as the knee was not improving after about 8 months, hobbled off for an MRI. Advanced patellofemoral arthritis in the knee, apparently – first time I’ve been advanced in anything. So began a regime of physio exercises for my knee. My knee continued to be painful, swollen and inflamed, and in July 22 I had the first ‘oil change’ – fluid drained off and an injection of something looking like Castrol GTX. Not a comfortable thing, but quickly done and to some degree it alleviated symptoms. After resting a few days physio exercises continued but four months later the knee was still bad, so I had to go in for another ‘oil change’. This time, symptoms were only alleviated for a week, and back I went to ask about seeing a knee surgeon for an opinion. At this point the doctor was discouraging: ‘you’re very young to have a knee replacement’ (thank you, all compliments welcome) … ‘and if I were you I wouldn’t go anywhere near a knee surgeon’. Well, my knee and my choice, and as I couldn’t walk for more than about 15 minutes I decided that was what I wanted to do.
Prep & Prehab
I still worked hard on my physio exercise, and Catherine Huck, Clinical Yoga specialist at tops:health Oxford, gave me clinical yoga exercises to help me get as strong as possible in my legs and in the muscles around my knee. I also started intermittent fasting, having read that each additional kilo weight you carry is multiplied about 3.5 times as weight bearing on your knee. If you’re able to choose your surgeon, look online at the National Joint Registry, which will give you lots of information about surgeons, the number of knee replacements done (the more, the better) and outcomes. I went to Sam Rajaratnam, a well-known and highly regarded surgeon in London because if I was going to have a knee replacement not only did I want an excellent surgeon, but equally important was knowing I would be in an excellent hospital with first rate nursing care. Because I’m worth it.
Another MRI and a series of X-Rays confirmed stage 4 osteoarthritis in my knee, and the surgeon sat with me and explained why I would need a total knee replacement (TKR) as opposed to a half knee replacement; when it was done would depend on how badly it was affecting my life and wellbeing, but I would need it done in the next few years. It would take 6 months to feel 90% recovered, a full year to feel 100%. A wise friend who had also had a TKR once said (a few times, actually) walk into summer rather than winter. Very good advice: the idea of recovering from a knee replacement and walking on icy pavements wasn’t appealing and it helps to wear light, loose clothing, so I booked in for my TKR in May.
Prehab physio exercises continued, and equal effort made at clinical yoga – a short 10 minute routine at home 4 days a week, and a 45 minute session once a week, to practise yoga safely and with control overseen by Catherine who as a physio could rein me in when needed (I’ve always been a ‘well if it’s not hurting I’m not pushing hard enough person’ which has probably contributed in no small part to the knee problem). Lesson learned. The hospital had given me a sheet of exercises to do after surgery, to start practising them in advance. Pah! Easy peasy, I thought (little did I know!). But it turned my mind to getting ready for surgery – just a few weeks away, now, and what I needed to prepare. I’m a self-confessed control enthusiast, so first and foremost were the household handover notes (what to do and how it must be done – no shortcuts allowed) printed off and stuck on the fridge. The hospital physio also told me to get a rubber shower mat so that there is no chance of slipping once I got home. I also got those big suction handles to affix to the shower wall and by the loo. A few more tips: a long-handled sponge (you won’t be reaching to wash your feet without one!), and a LimbO waterproof full leg protector (basically a leg-shaped shower hat which enables you to shower and protect the dressing after surgery). All of these were so useful and I’d recommend them to anyone who is going to get knee replacement surgery. The final thing I did was to book the hire of a Game Ready cryotherapy machine. This is a machine that takes ice cubes and is connected to a sleeve which wraps around your knee to ice it. I definitely couldn’t have coped well without this when recovering at home. It’s also used by elite athletes and at the LTA Wimbledon Championships so would bring me nearer to becoming the Olympic champion lying dormant in me all my life. Game Ready will deliver it to your home and have it collected. I had it delivered to a post-operative care clinic in Surrey, The Clavadel, where my surgeon had recommended I go to for 5-6 days after I was discharged from hospital. They would look after me while I was at ‘peak grumpiness’ after hospital.
The most important prep – book your physio appointments! The surgeon told me to have physio a few times a week for the first month, and to continue physio based on physio assessment. So, only one port of call: Dom at tops:health Oxford, who knows his onions, and his knees. All appointments booked in advance for the first four weeks I’m back home.
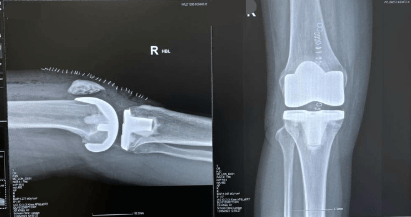
The TKR
So, I was going to have a Zimmer Biomet Persona Knee fitted, and off to hospital I went. A chat with the anaesthetist, a chat with the surgeon, then down to theatre (cold in there!) for a whiff of general anaesthetic and an epidural, and lo and behold I’m awake and ‘back in the room’ with a cryotherapy machine around my leg on auto, antibiotics on a drip and local anaesthetic fed into my knee at intervals during my three day hospital stay. I didn’t really feel any pain thanks to the cryotherapy and local anaesthetic, and next day the physios were getting me out of bed and walking up and down the corridor with a walking frame … very, very slowly. All was fine, I had a shiny new bionic knee, and on the third day my husband collected me to take me to the post-op care clinic. It was a Sunday, so traffic from central London to Guildford not too bad, but still not a comfortable journey … at all! I was very brave.
TKR +1 Week
I’ll include a little here on The Clavadel because it was a really helpful bridge between hospital stay and recovery at home. The Game Ready had been delivered ready for me (although there are lots there, hiring one myself meant I could keep it in my room and have use of it whenever I needed it). The nurses and carers are excellent and every day you have one hydrotherapy session and one physiotherapy session. If you are able to consider a stay here I’d recommend it – at this stage post surgery I was worried about how I would manage stairs, crutches, pain, sleeping, etc. so an understanding nurse was a better option for me than an exasperated husband. I did, however, choose not to join the evening talk on the history of Surrey villages (with slides). Every day the physio session would take measurements of my knee flexion and extension (bending and straightening) and those physio exercises I was given pre surgery at the hospital looked as though they would be impossible. I couldn’t lift my leg at all (and couldn’t for 12 days after surgery). The hydrotherapy was a gamechanger and gave me a headstart on my rehab. The pool there could lift and drop, there was a chair to sit in so I could bend my leg in the pool, and there is a pool treadmill, so I got a lot of encouragement by being able to bend my leg (nicely dry and encased in my LimbO protector). After a few days I was helped to start going up and down stairs – maybe other people are quicker to start this, but I was learning to trust myself and go at my own pace, not the alpha male bombing up and down the corridor one day post surgery (he suffered the next day; Schadenfreude). Recovery starts to feel tough as you start to move around more and physio gets working, and medicine gets reduced a week post-surgery. I was away from home, my husband was at work, and once or twice I just cried. I now understood what the surgeon had meant by ‘… it’s major surgery’. It’s a big thing for your mind, as well as your body, to countenance. You will have pain; TKR is basically elective assault so breathe, accept and work with it. Again, the clinical yoga and physio prehab proved invaluable.
Home and Rehab
Back home (a painful but slightly easier journey with a couple of stops to get out and walk and move a bit). A stool with my leg propped on it, and my best friend the Game Ready wrapped around my knee to use 4 or 5 times a day. I am much happier. Miraculously, the plastic tubs you get a Chinese Takeaway in are a perfect size to freeze water and fill the Game Ready ice chamber with a big block of ice. I have chow mein’ed my way through rehab and saved repeated purchases of bags of ice. I have also installed a Bell App on my phone – I can alert my husband to answer all my needs for ice cubes, pillows, cake or wine. It has a butler bell sound, cymbals, a cuckoo clock, sirens and loads more. I think my husband finds it annoying. I love it.
I managed a 10 minute walk on my crutches. Slow and very careful, watching for uneven paving as I was terrified of falling. Surprised how tiring it is. I have a pillow under my leg (lengthways) at night and have to lie on my back like Dracula, to sleep. The muscles have been cut so my knee is not supported if I lie on my side, so lying on my back listening to snoring is what it’s going to be for a while. Over the first weekend home my upper leg was quite swollen, but the hospital told me to expect flare-ups from time to time and I shouldn’t worry. I have a swollen, very bruised thigh and a very swollen knee which hates the surgical stocking I have to wear for the first two weeks, but I curbed the worry as I’m due to go to TOPS on Monday. I do the physio exercises as best I can, sitting on the bed and trying to flex my knee – another recommendation is to get a physio sliding disc to rest your heel in to help you slide your leg up and down, which it won’t on a bed, and there was no way I was able to get on the floor to do these exercises. I need help to get my leg lifted on to the bed, to use the Game Ready, to sit down: everything is difficult or not yet possible on my own.
Physio at tops:health
And lo, the hard work began. I saw Dom for my first appointment where he assessed my knee. It still has its dressing but I was taken through exercises and Dom measured flexion and extension and prescribed exercises, and when to do these and how often to use the Game Ready. Dom reassured me about the occasional flare-ups I should expect. I needed to keep working at the exercises and need to push into them a bit. So it was Groundhog day for the rest of the week: physio-push-pain-rest. I kept going for a little walk, which slowly gets a little easier, and was helped by beautiful weather and plants and flowers coming into bloom. This does help – rehab is boring, painful (but reasonably) and lonely, so find the joys of small things. At the end of the week, two weeks after surgery, I’m back to London town to get the dressing removed. The surgical stocking is off, then the dressing, then the nurse takes out all 30 metal staples from my knee. Not pleasant, but not too bad. Now my knee was revealed in all its new glory, save the stitches which look like an earthworm stuck on my knee. Ugh. The surgeon was with me too, and said my biggest challenge would be sleep, so I should rest and have the calories. He was also very clear that recovery of range and movement should be fast, and building back of muscle should be slow.
Lack of sleep was certainly my biggest challenge over the first two months. I woke up with the slightest shift as it would hurt. I suspended my intermittent fasting as I needed the energy, and three square meals a day definitely helped me. I continued seeing Dom three days a week, and this really helped me. It can be scary to push into the exercises: what is ‘ok’ pain, what is pain I should be concerned about? Having Dom’s supervision on exercises and his reassurance about pain really helped. You find the rehab is an iterative process – the bursa below my knee started hurting at 4 weeks post op, as I was working harder on split squats – I found that some things were too much and my knee flared up, so we left those to reintroduce them at a later date.
Other things I found I could manage very quickly. At 4 weeks post op I was unable to do a full rotation on an exercise bike, but at 5 weeks I could. The lack of sleep was, indeed, my toughest challenge for two months. Some days I’d come into my physio appointment trying not to cry, through sheer exhaustion. The pain itself is fine, really – it’s part of progress. Dom would measure flexion and extension and monitor this over the weeks. Some days it would be a little less or the same as before, but gradually the knee was bending a little bit more. Progress is in tiny increments so without these measurements it’s difficult to feel you’re progressing at all.
At 6 weeks post-surgery I went back to hospital for a final appointment with the surgeon and his head of nursing. Unfortunately, Dom and I had introduced an exercise to try a step down on my knee, but it was too early and my knee had flared up and was sore. The surgeon told me again – ‘range and movement first; you have years to build up muscle.’ Now the stitches had healed I could start treating the scar. I bought a product called SilDerm, a silicone gel which will reduce redness and flatten the scar over time. It’s worked brilliantly. I was at this point using one crutch just as occasional support – swelling made my knee give way sometimes when I walked a little too fast, so the crutch helped stabilise me. This gradually subsided but I still took a crutch with me when out and about amongst lots of people, as it alerts people to steer clear of you. The crutches were dispensed with completely by 8 weeks post op.
How It’s Going
I recall the surgeon’s guidance of the recovery timescale: ‘At 6 months you should feel 90% better, and it will take a year to feel fully recovered.’ I’m almost at 6 months now and feel I’m right on track. Okay, now swelling has gone my upper leg looks like one of those sad little shrivelled balloons you find behind the sofa 5 months after a birthday party, but my knee is good rate of progress is getting faster. From 100 degrees flexion one week after surgery, to 130 degrees at 9 weeks and 134 degrees now, Dom and I have pushed, repeated, measured and monitored over these five months since surgery. I’m back at the gym on the exercise bike and treadmill (doing only what Dom has prescribed) and gently starting some yoga exercises before I get back to yoga next week.
At tops:health, the rehab has incorporated three strands of care:
The reassurance during rehab that you’re actually doing great when you feel you’ve gone backwards, when you haven’t slept, when it feels as if the surgeon has just replaced your knee with a coconut, when you’re worried that something is wrong
The benchmarking and measurement which is reassurance in itself: seeing how far I could turn the wheel on an exercise bike, tracking balance distribution doing squats on the VALD ForceDecks, and measuring leg strength variance on leg extension
The physio exercises which are tailored to you and how you are progressing, plus soft tissue massage. Health ownership is key – it takes time in your day but you won’t get better unless you do the physio, and what’s the point of the surgery if you don’t do the work to get your knee back? What’s more: Dom will know (he has the eye of Sauron)
A long journey but feeling myself again with the expertise, care and kindness shown me at tops:health. A TKR is a lot to consider, prep for and recover from – it’s big, and requires work, resilience and patience. It was definitely worth it for me, and I hope this account helps give an insight into what you may expect.